People wait in line at a testing site to receive a free COVID-19 PCR test in Washington, D.C. On Monday, the CDC announced that people can isolate for five days, instead of 10, after they’ve tested positive for the coronavirus and have no symptoms.
Anna Moneymaker/Getty Images
hide caption
toggle caption
Anna Moneymaker/Getty Images

People wait in line at a testing site to receive a free COVID-19 PCR test in Washington, D.C. On Monday, the CDC announced that people can isolate for five days, instead of 10, after they’ve tested positive for the coronavirus and have no symptoms.
Anna Moneymaker/Getty Images
More than 200,000 people are testing positive for COVID-19 in the U.S. each day. Until this week, a positive test meant you should stay home for 10 days to avoid infecting others. Now, those who don’t have symptoms after five days can go back to their regular activities as long as they wear a mask, according to updated guidance from the Centers for Disease Control and Prevention.
The change in guidance released Monday was “motivated by science demonstrating that the majority of SARS-CoV-2 transmission occurs early in the course of illness,” according to the CDC.
CDC director Dr. Rochelle Walensky says the change was also motivated by economic and societal concerns. “With a really large anticipated number of cases [from omicron], we also want to make sure we can keep the critical functions of society open and operating,” she told NPR on Tuesday. “We can’t take science in a vacuum. We have to put science in the context of how it can be implemented in a functional society.”

Public health experts say a shorter isolation period may be reasonable at this point in the pandemic, but they say the agency’s new guidance is problematic because it relies on people’s self-judgment to assess their transmission risk — and could lead to more spread and more COVID-19 cases if people aren’t careful.
“The CDC is right. The vast majority of the transmissions happen in the first couple of days after the onset of symptoms … but the data shows that about 20 to 40% of people are still going to be able to transmit COVID after five days,” says Dr. Emily Landon, an infectious disease specialist at UChicago Medicine. “Is that person [leaving isolation after five days] really safe to carpool with or have close contact with or have them take care of your unvaccinated kids?”
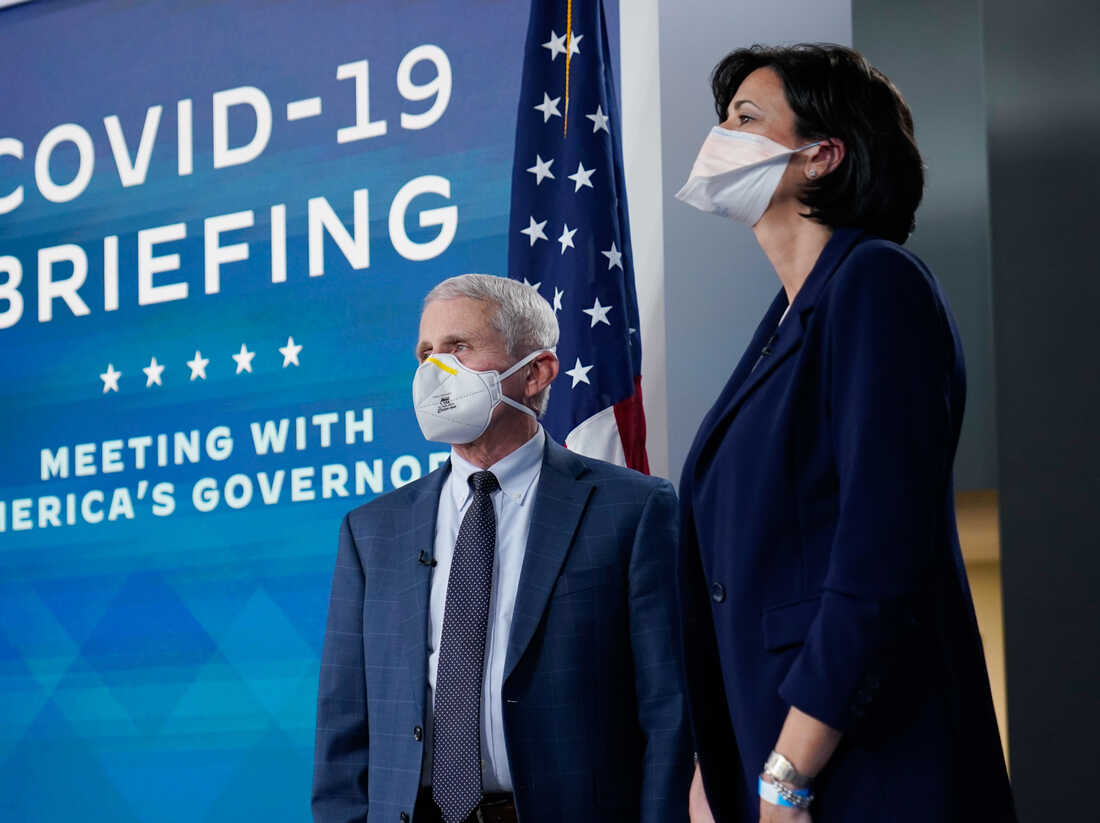
Dr. Anthony Fauci, who is the White House chief medical adviser and director of the NIAID, and Dr. Rochelle Walensky, director of the Centers for Disease Control and Prevention. Walensky defends the new CDC isolation and quarantine guidelines, saying she “trusts” the public to follow them.
Carolyn Kaster/AP
hide caption
toggle caption
Carolyn Kaster/AP

Dr. Anthony Fauci, who is the White House chief medical adviser and director of the NIAID, and Dr. Rochelle Walensky, director of the Centers for Disease Control and Prevention. Walensky defends the new CDC isolation and quarantine guidelines, saying